On the Mission to Unleash the Full Power of ICB in Cancer
Through immunotherapies utilising Immune Checkpoint Blockers (ICB), advanced solid cancers can today be treated with unprecedented efficacy. However, not all patients respond positively to these treatments. InFLAMES researcher, Docent Carlos Rogerio Figueiredo and his team are working to uncover the underlying causes of this resistance to ICB. They focus on patients suffering from malignant melanomas and lung cancers as main research models.
“Our ultimate goals here are twofold. Firstly, we want to be able to predict which patients can benefit the most from ICB treatment, in order to maximise the clinical assertiveness of this approach. And secondly, we’re striving to develop new therapies that can work synergistically with ICB treatments to overcome resistance, ultimately leading to better and more sustained responses for cancer patients,” Dr Figueiredo says.
Conventional cancer therapies are designed to attack the duplicating cells, mainly by targeting the DNA or some other target typical for in cancer cells. The problem is that normal cells that also duplicate can suffer from these treatments since they are incapable of exclusively attacking cancer cells.
Therefore, side effects emerge the need to pause these treatments so patients recover, which is when the tumors will also recover. These treatments are still effective if the tumor does not change and side effects are tolerable.
Mutations are superpower of tumor cells
One of the major challenges in dealing with cancer is the genetic instability of tumor cells.
“It means that they can acquire new mutations that help them to resist these treatments. These mutations can give the cancer cells a functional advantage in their ability to survive and multiply, making it more difficult for treatments to be effective,” Figueiredo explains.
Carcinogenic processes trigger cancer cells anytime in our lives due to various causes, including environmental carcinogens, inherited mutations, or lifestyle. Despite the risk of developing cancer at any point, we are relatively resistant to it thanks to our immune system, which constantly monitors our body and eliminates any newly transforming cancer cells.
ICB treatments reinvigorate immune cells
In a slightly different manner than cancer cells, our immune system can also adapt to changes.
“Therefore, ICB immunotherapies are not actually intended to directly attack cancer cells. What they do is they reinvigorate certain immune cells that have the ability to adapt to the changing nature of tumors. This method instills a sense of memory and adaptability to these tumors, thereby preventing their recurrence.”
As a result, cancer cells can find new ways to resist this treatment. For example, tumors may strategically obstruct the body’s ability to produce new antitumor T cells, which are the target of ICB immunotherapies.
This process is very complex and not yet fully understood, making it a challenging obstacle, Figueiredo says. He explains that the primary objective of the research conducted at his Medical-Immuno-Oncology Research Group (MIORG) is not only to comprehend but also to create successful interventions that can reverse this intricate process.
The findings give reason to test old drugs
MIORG has recently unlocked new findings that explain how some cancer cells can effectively modulate the metabolism of the tumor microenvironment, ultimately suppressing antitumor immune cells. The group identified existing drugs that could be used to reverse this process and be considered in new clinical trials in combination with ICB, to overcome resistance.
These findings were recently published in the Journal of Pathology, one of the most prestigious journals in the field of Pathology. The study was jointly conducted by Eleftheria Maranou, a doctoral researcher, and Maisoon Mattareed, a medical MRes student.
Moreover, the group implements powerful computer science tools to efficiently combine and analyse large datasets from clinical trials testing ICB, creating new methods that, in combination with their extensive knowledge of functional immunology, unlocked a new mechanism of resistance to ICB that was previously difficult to identify.
The future: better identification of patients
The group found that refractory or relapsing patients to ICB have deficient generation and activation of another effector immune cell, known as natural killer cells and T cell (NKT), which has a crucial role in fighting against cancer in response to ICB therapies.
The research was conducted by the Doctoral Researcher Mona Meng Wang, and were recently accepted for publication in Frontiers in Immunology. The group has also conducted a thorough review of the literature on how cancer cells evade responses to ICB by eliminating effector immune cells from tumors in a process called “cancer immune desertification”. This review will soon be available in the British Journal of Cancer.
Dr Figueiredo predicts that the next decade of immune checkpoint therapies will involve the rational development of new combinations with ICB, and the discovery of biomarkers that identify patients most likely to benefit from ICB.
In the future, MIORG applies reverse translational research together with Auria biobank and FICANWest clinicians to accelerate drug development in the Institute of Biomedicine, supported by the Faculty of Medicine, and funded by Academy of Finland, Sigrid Juselius Foundation, JAES Foundation, and InFLAMES.
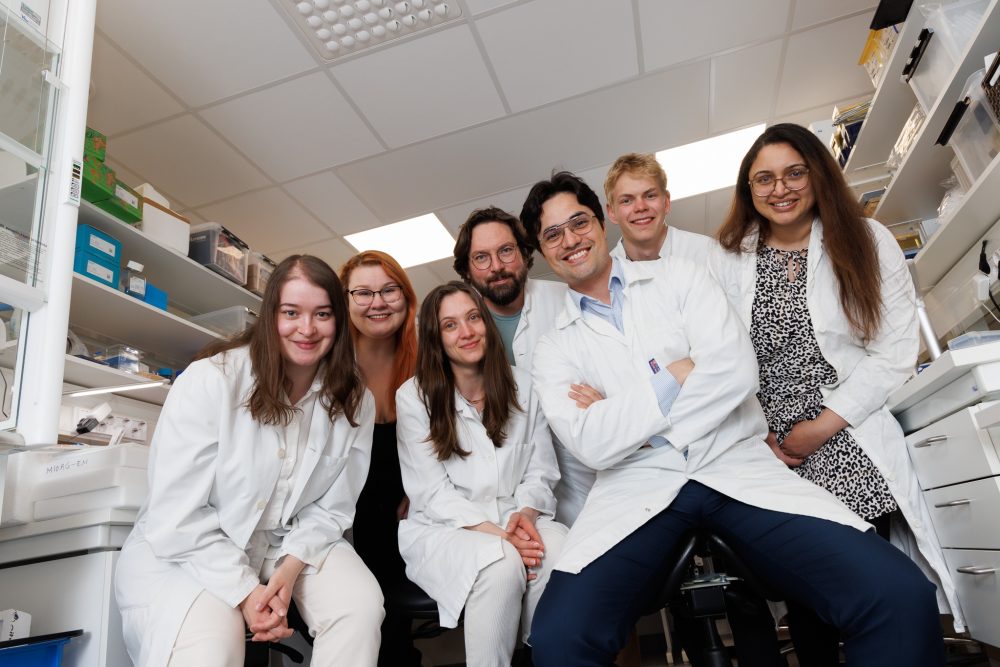
MIORG researchers are (from the left) Eleftheria Maranou (Doctoral Researcher), Saara Koskela (Doctoral Researcher), Miriam Langguth (Master’s student), Otto Pulkkinen (Computational Scientist), Carlos Rogério Figueiredo (Team Leader), Oskar Elenius (summer student) and Arfa Mehmood (Project Specialist).
.
